How does trauma and toxic stress impact the children we serve and the services we provide?
We all know that during the critical period of early childhood development (0 – 3 years of age), a child’s brain is most plastic…such that the environment and relationships with adults can significantly impact neural development.
These experiences in early childhood create a foundation for lifelong health, positive social relationships, academic success, and economic self-sufficiency into adulthood.1 Trauma can be a critical factor for why children we work with require our service, or why they are not progressing as expected.
Research shows that trauma experienced in childhood negatively impacts the physical, mental, social, and emotional development of children. Trauma is considered a critical public health issue impacting the health of children throughout the lifespan.2
Children who experience a high number of adverse childhood experiences(ACEs) are at greater risk for developing chronic diseases and health risk behaviors into adulthood. Chronic toxic stress impacts the developing brain in children and is linked to poor health outcomes and poor academic achievement.
In order to provide the most effective and comprehensive care, increased awareness of trauma and toxic stress is necessary for promoting positive health outcomes to children and their families.
|
What is Trauma? |
|
| Trauma defined by SAHMSA3 | Remember these 3 points |
| “events or circumstances experienced by an individual as physically or emotionally harmful or life-threatening, which result in adverse effects on the individual’s functioning and well-being” | · Event
· Experience · Effects |
The Adverse Childhood Experiences (or ACEs Study) by Dr. Felliti and others in the mid-1990s is the first study that identified the impact of childhood trauma on long-term health outcomes and overall emotional well-being.
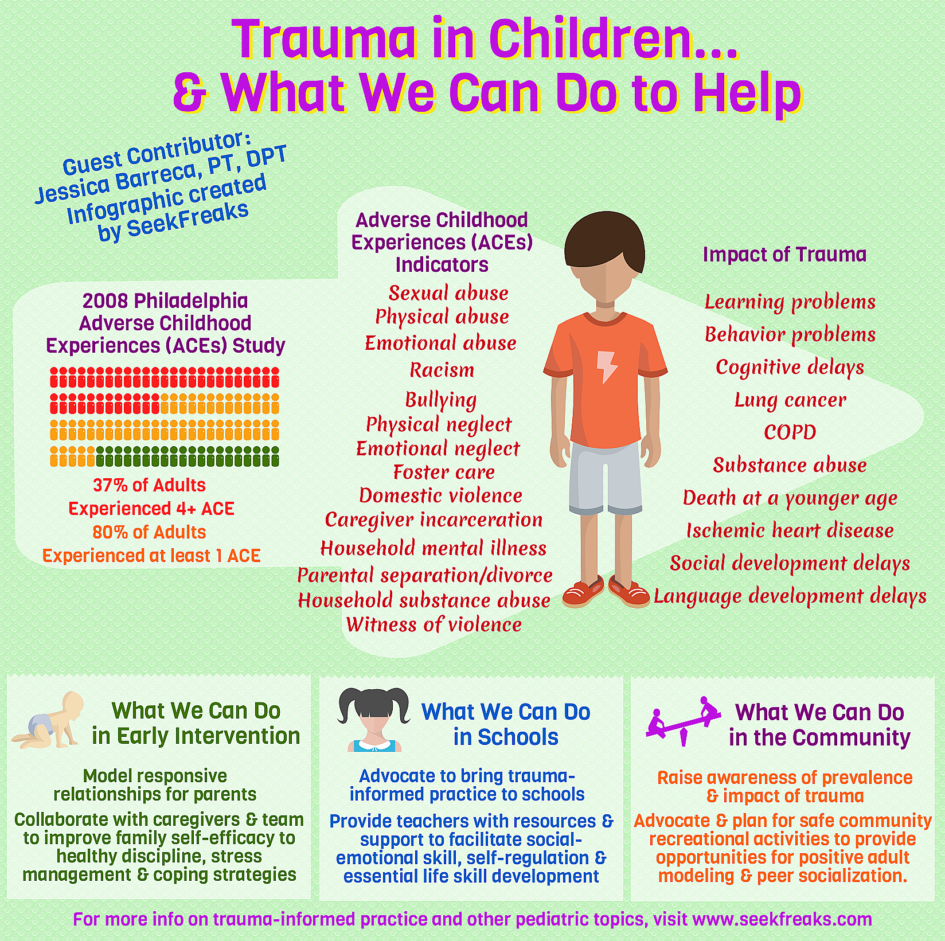
In collaboration with the CDC over 17,000 participants were asked questions about their own exposure to trauma during childhood such as neglect (physical or emotional), abuse (physical, emotional, or sexual) and trauma in the home environment (caregiver incarceration, domestic violence, household mental illness, parental separation or divorce, household substance abuse) and the related physical and mental health outcomes in adulthood. 4
|
How common is trauma? |
|
|
Original ACEs Study (1998)4 |
Philadelphia Urban ACE Survey(2008) 5 |
| Quick Stats to Remember:
· 50% of people have experienced 1 or more ACE(s) · 25% of people have experienced 2 or more ACE(s) Demographics: Primarily white, middle-class, adults with some college education (18+) |
Quick Stats to Remember:
· Over 80% of adults experienced 1+ ACE* · 37% of adults experienced 4+ ACEs* Demographics: Racially diverse sample of adults (18+); majority of participants had completed high school |
| *In addition to the 10 ACE indicators from the original study, questions on the following topics were added: Neighborhood Safety, Racism, Bullying, Witness Violence and Foster Care
ACEs are incredibly common and occur in children 0 -18 across all races, socioeconomic groups, ethnicities, and geographic regions but children living in poverty are at a higher risk for experiencing ACEs.5,6 |
|
Chronic Trauma such as abuse, neglect and/or living in poverty has a cumulative effect on a child’s development. Although stress is a normal and essential part of a child’s development, when young children experience persistent stress without adult intervention to mitigate these effects, the stress response system remains activated.7 This prolonged activation of the stress response system results in changes to the developing circuitry of the brain, immune and endocrine systems.2

Source: https://developingchild.harvard.edu/science/key-concepts/toxic-stress/
How does trauma impact the health and wellness of children?
- 90-100% of children with 6 or more risk factors (i.e. maternal depression, poverty) demonstrated delays in cognition, social, and language development at 3 years of age8
- 51% of children who self-reported an ACE score of 4+ had learning and behavior problems versus 3% of children who self-reported an ACE score of 0.9
- Individuals who reported 6+ ACES on average died 20 years before their peers who reported zero ACEs.10
Key Points to Remember
- As the number of reported ACEs increases, an individual’s risk for chronic health conditions such as ischemic heart disease, depression, lung cancer, and COPD increases.
- With an increase in reported ACEs, an individual’s health risk behaviors for smoking, substance abuse, obesity, and sedentary behavior rise.
To address the complexities of trauma and toxic stress, an interprofessional collaborative approach is key. What can SLPs, OTs, and PTs working with children and their families do to address trauma and toxic stress?
In Early Intervention
- Model responsive relationships for parents in order to foster social-emotional development, reciprocal communication, and safe physical exploration of the environment.11, 12
- Collaborate with caregivers, EC teachers, and other team members to improve child and family self-efficacy related to healthy discipline, stress management, and positive coping strategies. 13
In Schools
- Advocate for bringing trauma-informed practices to your schools and districts. 3
- Provide teachers with resources and support to facilitate social-emotional skill, self-regulation, and essential life skill development in children 11,12
In the Community
- Raise awareness of the prevalence and impact of trauma and toxic stress on children. 3
- Advocate and plan for safe recreational activities in the community to provide opportunities for positive adult modeling and peer social interaction.
Bottom Line: Our goal is to help parents, caregivers, teachers, administrators, and colleagues develop capacity to break the cycle of trauma.
Advocate for bringing trauma – informed practices to your schools, clinics and communities through the Four R’s of Trauma Informed Care3
- Realize the widespread impact of trauma and understand the potential paths for recovery.
- Recognize the signs and symptoms of trauma in patients, families, communities, fellow students and staff, and others involved in health care and education.
- Respond appropriately to fully integrate knowledge about trauma into policies, procedures, practices, and personal behaviors.
- Resist Re-Traumatization of patients as they engage with the health care system or individual providers.
Guest Contributor
Jessica Barreca, PT, DPT has over 15 years of working with children in a variety of settings including outpatient, early intervention and school systems. As an administrator in the special education office in the Chicago Public Schools, she led a team of 170 PTs and OTs in over 600 schools. She is currently the Community Site Coordinator in the Center for Interprofessional Education & Research and an adjunct faculty instructor in the Program for PT at Saint Louis University. Jessica is an ambassador for Alive and Well STL and is passionate about spreading knowledge and awareness regarding the widespread prevalence and impact of childhood trauma on families and children in our communities.
Additional Resources:
Center for Disease Control – https://www.cdc.gov/violenceprevention/acestudy/
National Child Traumatic Stress Network: http://www.nctsn.org
Robert Wood Johnson Foundation – https://www.rwjf.org/en/library/collections/aces.html
Burke Harris N. How childhood trauma affects health across a lifetime. New York, NY: TED Conferences LLC; 2014 Sep. Accessed on June 1, 2017. Available at https://www.ted.com/talks/nadine_burke_harris_how_childhood_trauma_affects_health_across_a_lifetime
References
1) Shonkoff JP, Garner AS; American Academy of Pediatrics Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e246. http://pediatrics.aappublications.org/content/129/1/e232.full. Accessed July 10 2017.
2) Shern DL, Blanch AK, Steverman SM. Toxic stress, behavioral health, and the next major era in public health. Am J Orthopsychiatry. 2016;86(2): 109-123.
3) Substance Abuse and Mental Health Services Administration Trauma and Justice Strategic Initiative. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. Rockville, MD. Substance Abuse and Mental Health Services Administration Trauma. 2014. HHS Publication No. (SMA) 12-4884.
4) Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14(4):245–258
5) Public Health Management Corporation. Findings from the Philadelphia urban ACE study. Philadelphia, PA: Institute for Safe Families; 2013. http://www.instituteforsafefamilies.org/sites/default/files/isfFiles/Philadelphia%20Urban%20ACE%20Report%202013.pdf Updated October 23, 2103. Accessed June 1, 2017.
6) American Academy of Pediatrics. Adverse childhood experiences and the lifelong consequences of trauma. https://www.aap.org/en-us/Documents/ttb_aces_consequences.pdf Published 2014. Published 2014. Accessed June 1, 2017.
7) Center on the Developing Child at Harvard University. Key concepts: toxic stress. http://developingchild.harvard.edu/topics/science_of_early_childhood/toxic_stress_response Accessed July 3, 2017.
8) Center on the Developing Child. The impact of early adversity on child development (InBrief). http://developingchild.harvard.edu/wp-content/uploads/2015/05/inbrief-adversity-1.pdf Accessed June 1, 2017.
9) Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse Negl. 2011 Jun;35(6):408-13.
10) Brown DW, Anda RF, Tiemeier H. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37(5)389-96.
11) Florida State University Center for Prevention and Early Intervention Policy. Supporting infant and early childhood mental health in speech therapy. http://cpeip.fsu.edu/mma/therapist/therapist_resources.cfm Published February 26, 2016. Accessed October 1, 2017.
12) Florida State University Center for Prevention and Early Intervention Policy. Supporting infant and early childhood mental health in occupational therapy. http://cpeip.fsu.edu/mma/therapist/therapist_resources.cfm Published March 3, 2016. Accessed October 1, 2017.
13) Center on the Developing Child at Harvard University. Three Principles to Improve Outcomes for Children and Families. http://www.developingchild.harvard.edu Published 2017. Accessed October 20, 2017.