Written by Peggy Morris, OTD, OTR/L, BCP . Peggy is an OT with 30+ years
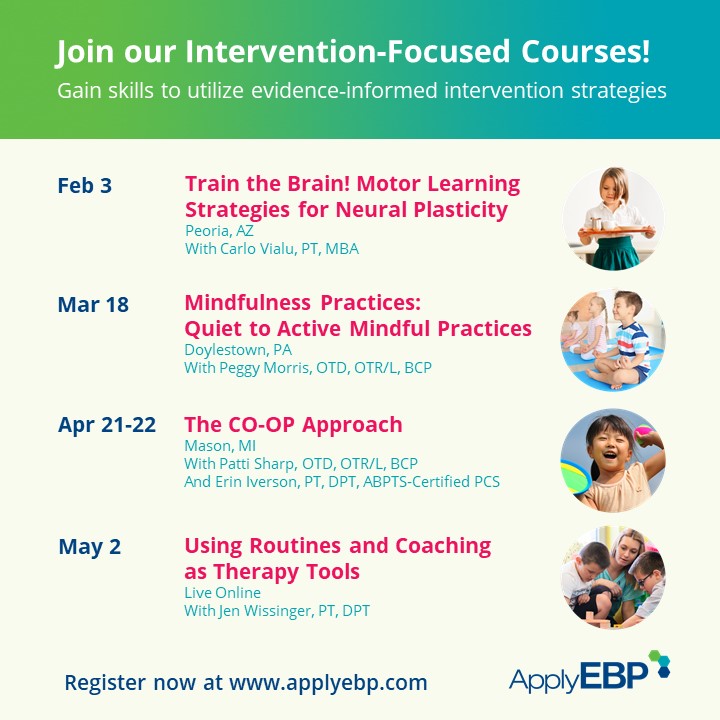
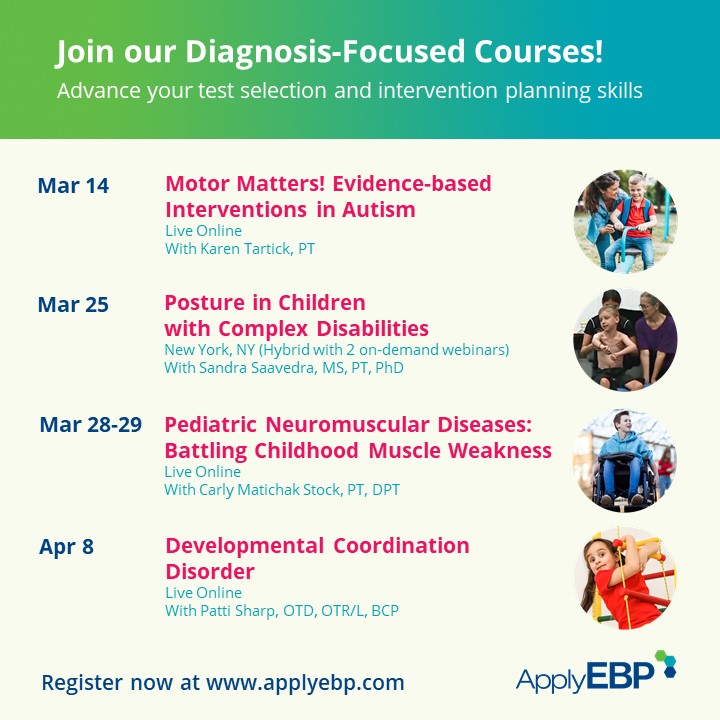
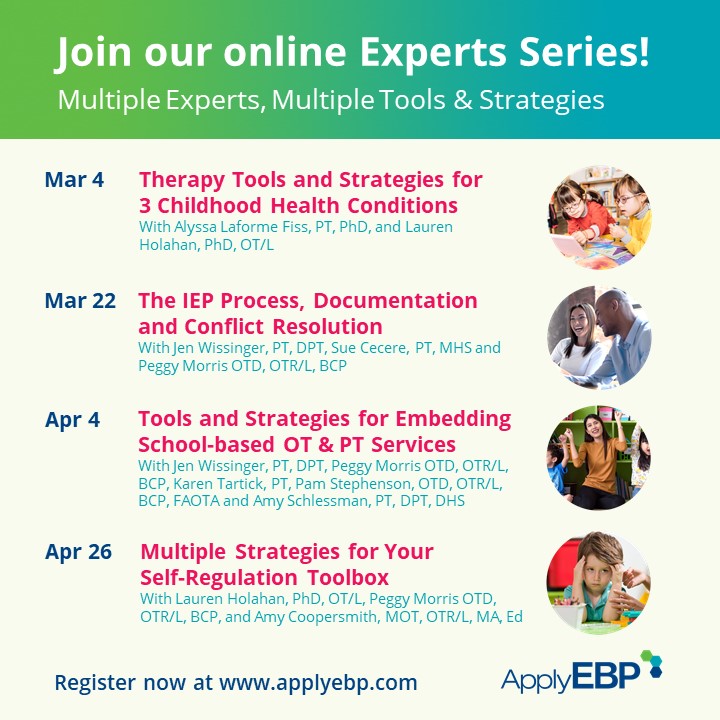
pediatric experience in early intervention, private practice, and out-patient services – but most of her experience and passion is in school-based practice. She teaches graduate students in the occupational therapy department at Tufts University, and man, do they keep her on her toes! She practices yoga, garden, and play golf for mental health and wellness. She presents evidence-based courses via Apply EBP. More information on these symposiums after the article below.
Fine Motor, Visual Motor/Perception 
Systems Approach to Handwriting 
Mindfulness Practices
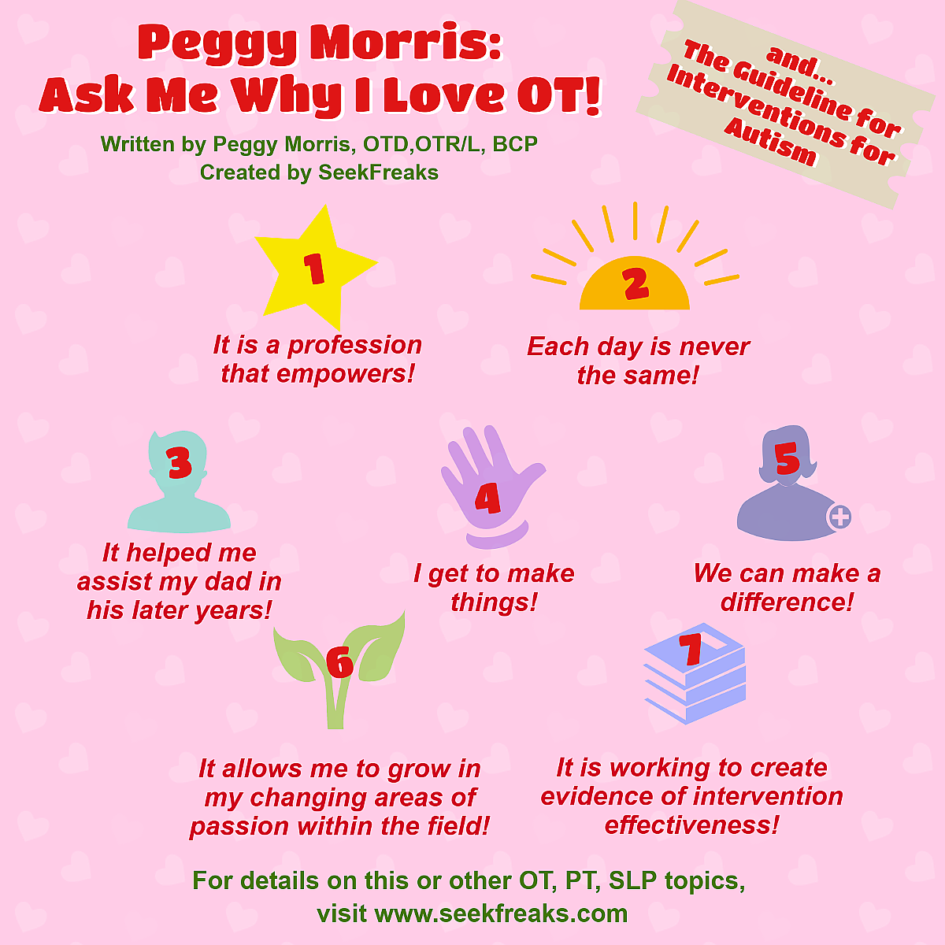
In this month of April, two of my many worlds collide, #AOTAinc and #LIUB. Yup, April is Occupational Therapy Month and Autism Awareness Month, two really important worlds to me. The American Occupational Therapy Association celebrates the profession of occupational therapy all month long; this year, one of their celebration themes is “Ask me why I love occupational therapy!”, so I thought I’d tell you! Hmmm…
- I love occupational therapy because it is a profession that empowers. It empowers me to think creatively to problem-solve for clients, and through OT, our clients are empowered to do the many things they want, and need, and have to do in their daily lives.
- I love occupational therapy because each day is NEVER the same! I crave, and thrive on, variety; OT affords me that.
- I love occupational therapy because it helped me to assist my Dad in his later years (he was a polio survivor).
- I love occupational therapy because I get to make things. OTs are the original makers. I get to use my hands to create something for clients to use; that is unbelievably rewarding. If you haven’t viewed this yet, check out this TedTalk by an OT on Making.
- I love occupational therapy because of the many different ways and places where occupational therapy can make a difference. The possibilities for work place environment in occupational therapy are amazing. We can work with children, or adults, or children and adults. We work across the life span, from the NICU to end-of-life care. We work in the most acute setting, say that NICU, and we can work in community-based settings, such as a public school or a mental health organization.
- And I love occupational therapy, because it allows me to grow in my areas of passion within the field, even as my areas of passion have changed, and still remain an occupational therapist. That is one sign of a wicked awesome profession! (I work in Bahston, in case you couldn’t tell)!
- I also love occupational therapy because it is working slowly and surely to create evidence of intervention effectiveness for our clients. One of the areas that has seen a significant growth in research is that of occupational therapy use with clients with Autism Spectrum Disorder. Ah, see where I’m going?! Tying both my worlds together?!
The American Occupational Therapy Association, in 2016, released Occupational Therapy Practice Guidelines for Individuals with Autism Spectrum Disorder. It is a publication that grew from the original practice guidelines, published in 2009 and focused on children and adolescents with autism, to incorporate a lifespan approach, as well as a strengths-based perspective.
In case you are not familiar with AOTA’s practice guidelines, and there are a few (autism, mental health promotion and prevention, and sensory processing in children to adults with low vision, neurocognitive disorders, and adults requiring home modifications, to name a few), these practice guidelines are, in essence, systematic reviews of current evidence on the topic.
This is music to the evidence-based practitioner’s ears! The authors of systematic reviews do all the heavy lifting for us. They find the relevant literature. They determine and rate its level. They check out the methodology. They review the statistical analysis. AND THEN…they distill it into practice recommendations: what to do, what not to do, etc.
If you are in a practice area for which there is a practice guideline, then a really easy way to head toward that best practice of layering in current evidence to your clinical reasoning and ‘gut instinct’, is to read a practice guideline.
The Guidelines for Interventions for Autism is about 100 pages long, excluding the appendices; so, it is not an easy read, but I think that best practice isn’t always as easy as we might want it to be! I would rather be in my garden than reading for work, usually any day of the week.
BUT, it is usefully organized into topic areas, such as interventions that focus on social skills and play participation, interventions that focus on work, ADL, and IADL performance, interventions that focus on family coping and resilience, and sensory integration and sensory-based interventions, so you can chunk it up.
AND, it comes with one of those handy-dandy, flat-as-a-pancake, looks-like-a-credit-card USB flash drives that holds searchable Evidence Tables. They made Evidence Tables! And shared them!!! Like I said, all of the heavy lifting.
Now, there are way too many findings to report on all of them for you in this post, but I can tackle a few that I hope might be really relevant for you right now. In the AOTA’s Practice Guidelines, qualifiers of strong, moderate, and weak are used for the analysis of evidence. Other qualifiers used include promising, limited, and mixed.
Let’s start with the strong. Peer group interventions, those that involve an occupational therapy practitioner using a curriculum or training program, either in a clinic or the child’s natural environment, shows strong evidence for improving social skills, including improved social competency, participation, and self-esteem. Also strongly supported by current evidence as being effective interventions are technologies to teach employment-related skills, specifically technologies including computer software, PDAs, video-modeling, and visual supports. Ah, visual supports! So this is the tricky part of EBP: strong evidence for visual supports for folks with autism when the outcome is improved employment-related skills. This is what we have evidence for, very specifically. As we layer in the current evidence to our existing practice, we then use our clinical reasoning and ‘gut’ to decide if we can safely extrapolate that research to a different outcome. I know I use visual supports outside of this employment-related skills outcome. EBP doesn’t mean we should abandon all visual supports used in other areas of intervention; BUT, it is on us, then, to determine its effectiveness for our particular client. Data collection is WAY outside the scope of this post, but data collection is how we make individual evidence.
On to moderate. Moderate evidence for effectiveness exists for interventions in joint attention training, specifically the JASPER (Joint Attention, Symbolic Play, Emotional Regulation) system. Sensory-based interventions (multisensory, not Ayres™ SI), were found to have moderate effectiveness for improved behavior and occupational performance for clients with autism. Moderate evidence exists to support use of behavioral techniques to improve RRBs.
There is limited evidence to support the use of physical activities, such as jogging or yoga, to promote student behaviors and classroom performance. This evidence is classified as weak, since there are only three studies. While the results of these studies are promising, more research is needed to build the evidence base. Similarly, interventions in the area of relaxation training and breathing for outcomes in coping, resiliency, and self-efficacy are limited in support of the practices. There is mixed evidence for the effectiveness of Ayres™ sensory integration, although moderately favorable for this type of intervention for improvement in individualized goals (think goal attainment scaling).
Of interest, there are two areas I want to touch on before we end. Single-sensory interventions (think ball chairs and weighted vests) are not supported by evidence. The research, at least that to date, for dynamic seating, does not show sufficiently strong evidence to warrant its recommendation. The evidence on weighted vests, in this population, is strong enough in the opposite direction, to discourage their use as a means for modifying behavior.
Phew, that’s a lot to digest, and it is only a portion of the systematic review that is the Guidelines for Occupational Therapy for Individuals with Autism Spectrum Disorder. It is an important document to assist therapists with heading toward better/best practices. Again, someone else did the heavy lifting, and we can reap the benefits, and so can our clients with autism. One last share: two case studies based on adolescents with autism spectrum disorder who are involved with occupational therapy practitioners, and receiving services guided by the Practice Guidelines.
So, celebrate Occupational Therapy month. Comment below why YOU love occupational therapy! Post a pix of something you’ve made in OT! Celebrate National Autism Awareness Month. Recognize the strengths and stories and community events geared toward those living with autism, as a way to educate those of us who are not. Now I am headed out to the garden, which in THIS April in New England, means coaxing the just-emerging crocus out of the snow and raking the leaves I never got to last fall! Enjoy the month!
Join Peggy and other evidence-based presenter at these courses…
References:
AOTA (2016). Occupational Therapy Practice Guidelines for Individual with Autism Spectrum Disorder. Rockville, MD: AOTA Press
Tomcheck, S. Koenig, K., Arbesman, & Lieberman, D. (2017). Evidence Exchange – Occupational therapy interventions for adolescents with autism spectrum disorder. American Journal of Occupational Therapy, 71, 7101395010. https://doi.org/10.5014/ajot.2017.711003











1 Pingback