SeekFreaks, a difficult transition for parents is when they leave the hospital with the bundle of joy and no procedure manual! For some parents, an early interventionist is more than helpful but actually feels like a life line. Then, just as things are smoothing out, here comes school? How can we ease the abruptness of this transition, you ask? By beginning early! Preparation should begin a year before, near the 2nd birthday and continues until a child is acclimated to and making progress in the new setting (8-12 weeks) after placement. To ensure things go smoothly for EVERYONE: families, children and providers, start preparing at 24 months. Here’s a list of the top 10 things to do before transition from Early Intervention (EI) to (SB) from a physical therapist’s perspective (me, Denise Swensen). SeekFreak OTs and SLPs, if you want to do a guest post from your disciplines’ view of this transition, here is a link with all the details to contribute a post! https://www.seekfreaks.com/index.php/interested-in-becoming-a-seekfreaks-guest-contributor/
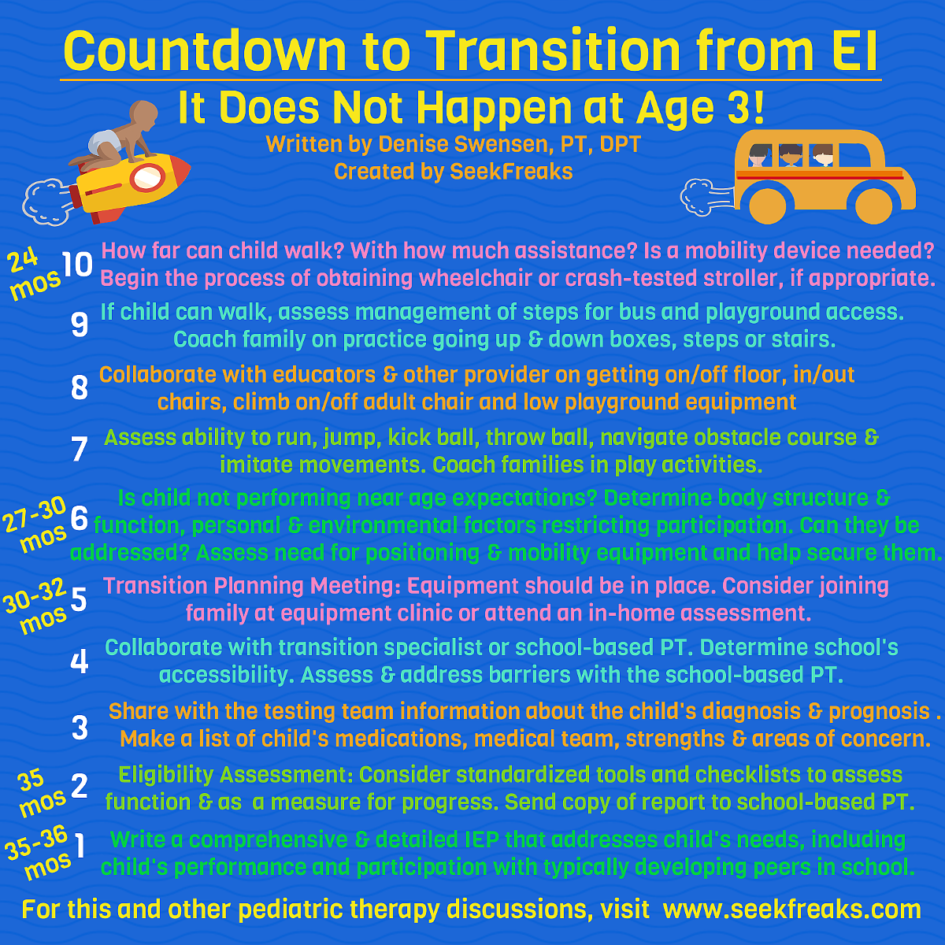
Countdown to Transition at 3
#10. At 24 months – Assess how far the child can walk and how much assistance he/she needs. If the child is not yet walking, use your clinical judgement to determine if the child will need a mobility device for travel on the bus and in school. If the child will likely be non-ambulatory or may only walk with an assistive device, (i.e. GMFCS Level III-V), begin the process of obtaining a wheelchair or crash-tested stroller. Either way, discuss with the family ways to acquire the device by either purchase or on loan. Add to the 24-month goal.
#9. At 24 months – If the child can walk, assess if he/she can manage at least 4 standard or higher steps for bus and playground access. If not, coach the family to start working on stepping in/out of various height boxes, on/off various height steps, and up and down short staircases. Add outcomes to the IFSP.
#8. Collaborate with educators and other providers to determine if the child can get on/ off the floor independently, in/out of child-sized chairs, climb low playground equipment, and climb on and off a firm adult chair. Add outcomes and a short episode of care by a PT to the IFSP.
#7. Assess the child’s ability to run, jump, kick a playground ball, throw a small ball, navigate through simple obstacle courses and imitate movements using songs that direct movement. Coach families in play activities to help with mobility, balance and coordination, turn taking and reciprocal play with an adult or peer.
#6. At 27-30 months – If the child is not performing near chronological age expectations, determine the underlying body structure and function limiting the child’s progress. Can it be changed with a short, intense episode of care? Are there other things such as personal or environmental factors limiting progress or participation? Can they be addressed? If there are limitations that affect the child’s ability to roll, sit independently, transition to standing, and walk, assess the need for positioning and mobility equipment including a bath chair, adaptive seating, stander and wheelchair or WC-19 adaptive stroller, if not already in place.
#5. TPM Transition Planning Meeting 30-32 months. Only 6 months to go! Equipment should be in place or at least on order as many times it takes 6 months (or more) to get equipment. Help families with resources for funding, loaner closets, donations, internet sources (Craig’s List, eBay) church groups (Rotary Club, Elks, etc). Consider going with the family to the equipment clinic or attending an in-home assessment to ensure the child gets child and family-friendly equipment that will be used daily.
#4. At 30 months – Collaborate with the transition specialist or the School-based PT. Determine if the school the child is most likely to attend is accessible. Encourage families to tour the facility where their child may be going. What environmental and personal factors are particular to the school? Assess barriers to participation with the receiving PT and come up with a plan to address these needs through Supplementary Aids and Services on the IEP.
#3. Gather information on particular diagnoses and share information with the testing team, parents (hopefully you have shared with the family already) and receiving teams (with parent permission) regarding symptoms, characteristics, prognosis and any other pertinent information. Make a list of outside medical professionals and providers the child and family are followed by, current medications, strengths and areas of concern. All this information is essential for a smooth transition between Part C and B providers.
#2. At 35 months Eligibility Assessment – Besides standardized assessments such as the DAYC-2, BDI-2 and PDMS (which may be required in some jurisdictions), consider other tools (standardized, criterion referenced or checklists) to assess function which can be used to measure of progress over time:
- Gross Motor Function Classification System (GMFCS)
- Gross Motor Function Measure (GMFM) (CP and Down syndrome)
- Timed Up and Go In Children (TUG-IC)
- 30-Second Walk Test
- Pediatric Balance Scale (PBS)
- Pediatric Evaluation of Disability Inventory (PEDI)
- Pediatric Evaluation of Disability Inventory-Computer Adaptive Test (PEDI-CAT)
- Early Clinical Assessment of Balance (ECAB)
- Segmental Assessment of Trunk Control (SATCo)
- MOVE: Top-Down Motor Milestone Test
- APTA Part C to part B Transition checklist
- Clinical Observations
- Record review
- Parent/Provider input
Identify barriers to participation based on the evaluation and assessment. Send a copy of your report to the receiving PT and parent and collaborate on goals and objectives that are important and necessary to the child and family for participation in regular school activities and routines.
#1. 35-36 months IEP. Write a comprehensive and detailed IEP that addresses the child’s needs, including activity limitations and participation restrictions related to the child’s performance and participation with typically-developing peers in school. Include bus and playground access, ability to retrieve toys in bins and on low shelves, hanging up coat and backpack in cubbies, toileting, hand washing and other personal care, transitions to other areas of the school, participation in PE or motor group, sitting for small group instruction, play on the floor, snack time, emergency egress and any other regular school routines and activities. For children with severe motor impairments, embed motor strategies (positioning and mobility) into pre-academic, self-help, or communication areas in the IEP.
Take-home points
- Start early.
- Collaborate with families, outside providers, service providers and the receiving school team.
- Be mindful that participation starts when the child steps foot (or wheel) on the bus and ends when they get off.
- Write a comprehensive transition report that describes the child’s motor abilities and needs so anyone who reads it gets a clear idea of what to expect.
- Don’t get stuck on gross motor The IEP is transdisciplinary and If possible write embedded goals for positioning and mobility under other areas of need, especially for children with severe motor impairments.
A successful transition is
- from an ecological perspective
- tailored to the individual needs of the child
- focused on promoting positive outcomes
- a successful adjustment both developmentally and socially in a critical time frame (Rous, 2006)
Reference
Rous, B., Harbin, G. & McCormick, K. (2006). A Child Outcome Framework for the Early Childhood Transition Process. Research Brief, September 2006, National Early Childhood Transition Center (NECTC) http://www.hdi.uky.edu/nectc/Libraries/NECTC_Research_Briefs/A_Child_Outcome_Framework_for_the_Early_Childhood_Transition_Process.sflb.ashx
About the Author
Denise Swensen, PT, DPT, is a physical therapist and transition specialist at Prince George’s County Public Schools and Judith P. Hoyer Early Childhood Center.