The author, Carlo Vialu, PT, MBA, is co-creator of SeekFreaks. He loves promoting function and participation for children and youth with disabilities, from our assessment to our interventions, via his continuing education courses with Apply EBP. More about these courses after the article.
PT COUNTS ( PT related Child Outcomes in the Schools)…the gift of a research that keeps on giving!
Laurie Ray and I covered the earlier papers from PT COUNTS by Chiarello et al, 2016 and Effgen et al, 2016 in our HeFreak Says, SheFreak Says article where we discussed these main takeaways:
- School-based PT works…yay!
- School-based physical therapists are providing more interventions within school routines than previously reported, and
- School-based physical therapists are generally good at prognosticating 1-year goals
So was I excited when this follow-up article came out: Chiarello, L. A., Effgen, S. K., Jeffries, L. M., McCoy, S. W., & Tezanos, A. G. V. (2020). Relationship of School-Based Physical Therapy Services to Student Goal Achievement. Pediatric Physical Therapy, 32(1), 26-33.
Extra Oomph! to Surpass the Goals
In this new paper, the authors wanted to “determine the relationship of [school-based] physical therapy services to goal achievement.” But since the students in the study, on average, achieved their goals, what they studied are service variables that differed between those students who surpassed their goals and those that just met (but not surpassed) their goals.
So you can think of these service variables as that additional oomph! That icing that makes the cake even yummier. That extra difference that we can provide to make our students’ lives even better.
Just a couple of disclaimers before you read our takeaways.
- Associations, not cause-and-effect: This is a paper on the association between variables (i.e., intervention strategy and surpassing goal), not a cause-and-effect. So you should closely monitor your student’s progress as you modify and align your goals and interventions to the results of this study and our suggestions in this article.
- There are lessons for all pediatric OT, PT and Speech practitioners here: This paper focuses on school-based physical therapists, but it is fairly easy to see how many of the lessons can be applied to all pediatric PT, OT, and Speech practitioners whether they work at home, in a clinic or in schools. So we will give some thoughtful points and questions on how the results of this study can help us all move our practice forward.
- Laurie Ray and I wrote a more succinct Clinical Bottom Line on this paper, and you should read it too!
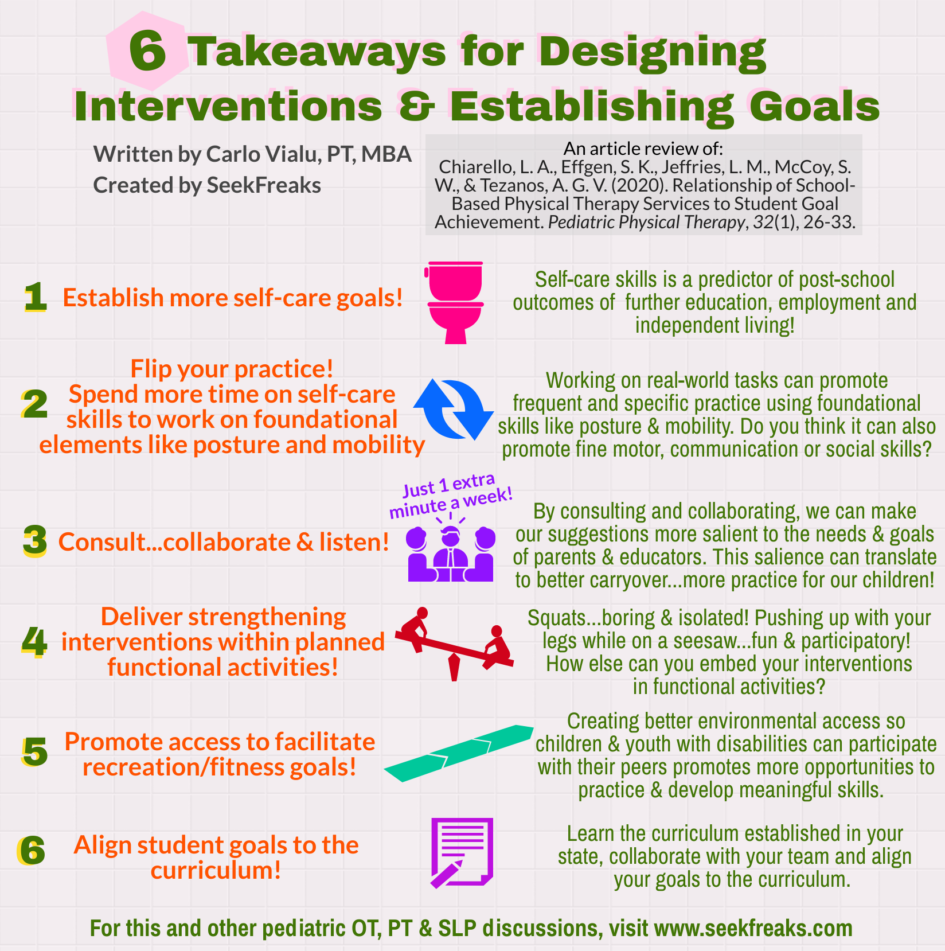
Here are our SeekFreaks takeaways:
Takeaway #1. Establish more self-care goals!
According to the study, school-based physical therapists established very few self-care goals!
Laurie and I lamented this in our HeFreaks Says, SheFreaks Says article. Why? We know that self-care skills is a predictor of success for our student’s success in gaining post-school employment, further education, and independent living (Read SeekFreaks’ 18 Predictors of Postsecondary Outcomes). So teaching self-care skills should not be ignored. In fact, it should be a priority!
This leads us to our second takeaway…
Takeaway #2. Flip your practice, and spend more time on self-care skills, to work on foundational elements like posture & mobility!
The study found that more time working on self-care skills is associated with exceeding posture and mobility goals!
Glass half-empty reaction: There’s the rub! If school-based therapists were working on more self-care goals, would more of their students exceed their posture and mobility goal expectations?
Glass half-full reaction: Work on real-life function and you may be hitting 2 birds with 1 stone…the real-life function (e.g., self-care), and the “foundational elements or skills” (e.g., posture and mobility).
As Patti Sharp, OTD, OTR/L discussed in her SeekFreaks article How a Cartwheel Flipped My Practice Right Side Up, many therapists are very comfortable with working on foundational elements or skills. I’ve experienced the same. Ask a random therapist why they are doing such and such activity, and one common answer is “I am working on the underlying skill to help him/her achieve ‘so-and-so’.”
On the same note, we may feel that by not addressing a foundational skill directly, we are not helping the child holistically. While the verdict on this is, at best, unclear, or, at worst, doubtful, I am glad that this study further supports that I don’t have to make a choice between real-life function and foundational skills.
Now, we can have our cake and eat it too! Work on functional tasks, and foundational skills employed in that task may follow. Let’s explore the possible reasons why working on self-care helped exceed posture and mobility goals:
- Self-care requires posture and mobility!
- Using the toilet, say, requires mobility to go to the bathroom and transfer skills to and from the toilet seat. It also reinforces assuming and maintaining postures. Standing posture to pull down or pull up ones’ pants, and seated posture and balance while toileting, for example.
- Washing hands require mobility to go from the bathroom stall to the sink, and holding one’s posture while washing and drying hands.
- Self-care happens frequently!
- Compared to direct therapy for posture and mobility that may happen a few times a week or month, self-care happens every day…in fact many times a day!
- Coaching educators and family members on strategies to develop toileting skills provides the child more opportunities to work on their posture and mobility. (More on this coaching under Take-away #3).
- Self-care incorporates lots of motor learning principles! (in addition to frequency just discussed)
- It is salient (i.e., meaningful) – we all have to go! And the ability to do one’s self-care independently is a great incentive in itself.
- It is specific – it is a real task, unlike, for example, being perturbed side to side while sitting on a therapy ball
For OT and Speech practitioners, how much opportunities for learning fine motor, communication and social skills can be developed during a self-care activity? For home-based and clinic-based practitioners, can you help create opportunities to practice self-care skills at home?
Takeaway #3: Consult…collaborate and listen!…to promote frequent practice of skills when they occur naturally.
Sorry, I can’t help the play with that Vanilla Ice classic line. (Now I can’t get it out of my head…and you’ll probably have the same problem too.)
The study found that more time spent on “services on behalf of a student” is associated with exceeding posture and mobility goals!
“Services on behalf of a student” is defined in the study to include consultation, collaboration and documentation. So now, can we finally pin even more value to the time we spend talking to teachers, other school personnel and parents!
It is likely that by consulting and collaborating, educators become better at supporting not just the development of classroom skills, but also, of posture and mobility.
Such consultation and collaboration may include coaching educators on self-care (as just discussed above), performing classroom/school activities, negotiating the school environment, and the like.
The same reason just listed in Takeaway #2 above applies…services on behalf of the student can provide frequent practice, specificity, and salience. And I would argue that by consulting and collaborating, we are better able to take into consideration and address the needs and goals of educators and parents…making our suggestions as salient to them as it is salient to the child/youth. And this salience can translate to carryover, i.e., more opportunities for practice.
Whether you are an OT, PT or Speech practitioner, create time to consult and collaborate with parents, teachers and other educators. Maybe you are thinking, but I don’t have time for that!!!
In this study, an additional 20 minutes of services on behalf of the student in a span of 20 weeks, was all that it took to increase the odds of exceeding the goal by 37%. Yes, just 1 extra minute a week…insert exploding brain emoji here!
Takeaway #4. Deliver strengthening interventions within planned functional activities.
The study found that greater use of functional strength as an intervention is associated with exceeding recreational/fitness goals!
We often associate fitness with strength. But not all strengthening programs are created the same. The PT COUNTS Training Manual differentiates 2 types of strengthening:
- “Strengthening using progressive resistive exercise (PRE): Strength-building exercises in which the student is required to work against increasing resistance, applied via external resistance”; and
- “Strengthening (Functional): Strength-building exercises or activities in which the student is required to work against increasing resistance or gravity, or to work eccentrically within planned functional activity.” (McCoy, S.W., Jeffries, L., Effgen, S., Chiarello, L. A., 2011
And, it is the latter (functional strengthening) that was associated with the children exceeding their recreational/fitness goals. So, let’s plan to deliver our strengthening interventions within planned functional activities (not separate of them). While the article does not provide examples of what the therapists in the study reported as functional strengthening, here are some of my thoughts:
- Instead of squats, how about asking the child to “spring” up their legs while on a seesaw
- Instead of chest press, how about asking them to push another child on a swing
Functional strengthening can make “strengthening exercises” more fun and participatory, instead of isolated and boring.
For all pediatric practitioners, this is also a reminder to work on body function and structure (or as difficulties in this area is called…impairments) in a functional manner – not in isolation. Strength, visual perception, vocalization, etc. in the real world do not happen in a vacuum. They are recruited by one’s body based on the requirements of the task, and the environment where the task is occurring. As Adolph and Hoch (2019) entitled their paper, “Motor Development: Embodied, Embedded, Enculturated, and Enabling.” (Yes, this is another great read!)
Speaking of enabling…
Takeaway #5. Promote access to facilitate recreation and fitness goals!
The study found that greater use of mobility for playground access as an intervention is associated with exceeding recreation/fitness goals!
If you can’t access the playground, how can you use it?
We all know that many playground areas are inaccessible for those with differing mobility. From the woodchip that may help cushion falls but makes it hard to use a walker or a wheelchair, to high playground equipment that are difficult to reach.
So, it makes sense that working on mobility to access the playground can create more opportunities for recreation, and therefore, help achieve (and exceed) recreational and fitness goals.
All OT, PT and Speech practitioners should think of creating better access for our children and youth with disabilities to participate with their peers, so they can have more opportunities to practice and develop all sorts of meaningful skills.
Takeaway #6. Align student goals to the curriculum!
The study found that school-based physical therapists established very few academic goals.
While I can hear the reasoning for this one, “we are therapists, not teachers”, let us not forget that as related services provider we are charged to support student’s education and preparation for postschool outcomes of further education, employment and independent living.
Here’s a great suggestion from SheFreak, Laurie Ray – learn the curriculum established in your state, and align your goals to the curriculum!
PTs, for example, can align recreation and self-care goals to support the Physical Education and Health curriculum. OT and Speech practitioners, which curricula can you support?
Better yet, you should also collaborate with your team to establish goals that ensure support access, participation and success in the student’s education!
Now it’s your turn to read this latest article from PT COUNTS, and tell us your takeaway by commenting below!
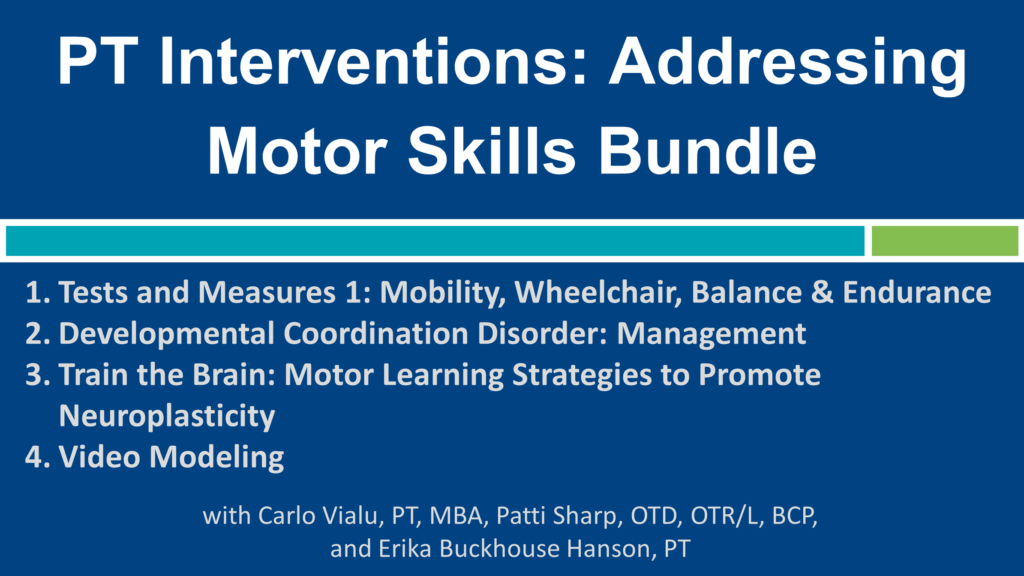
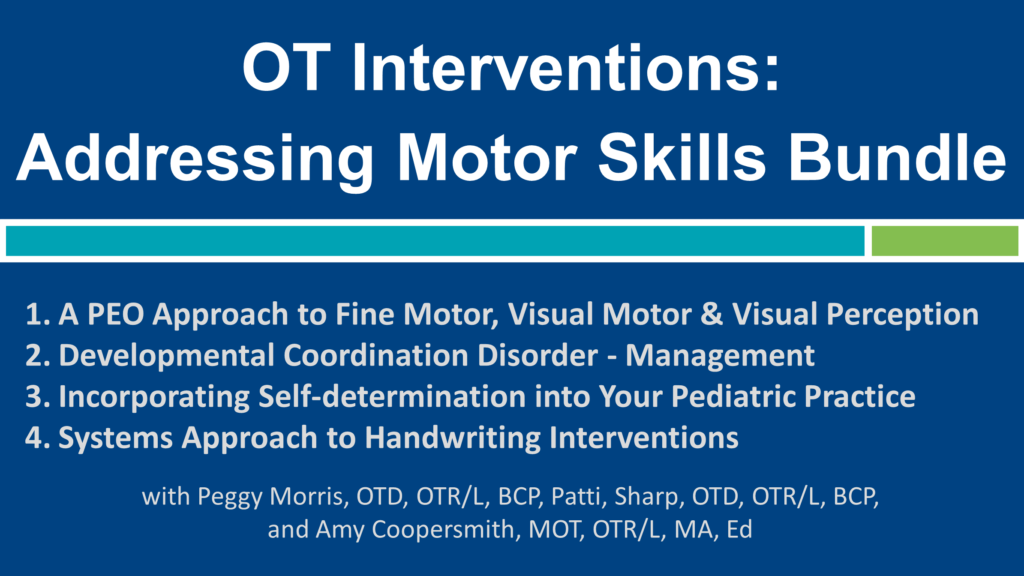
Join the author, Carlo Vialu and other school-based experts in…
Join Carlo Vialu and other experts at these all evidence-based, all practical continuing education courses:
References
Adolph, K. E., & Hoch, J. E. (2019). Motor development: Embodied, embedded, enculturated, and enabling. Annual review of psychology, 70, 141-164.
Chiarello, L. A., Effgen, S. K., Jeffries, L. M., McCoy, S. W., & Tezanos, A. G. V. (2020). Relationship of School-Based Physical Therapy Services to Student Goal Achievement. Pediatric Physical Therapy, 32(1), 26-33.
Chiarello, L. A., Effgen, S. K., Jeffries, L., McCoy, S. W., & Bush, H. (2016). Student outcomes of school-based physical therapy as measured by goal attainment scaling. Pediatric Physical Therapy, 28(3), 277-284.
Effgen, S. K., McCoy, S. W., Chiarello, L. A., Jeffries, L. M., & Bush, H. (2016). Physical Therapy–Related Child Outcomes in School: An Example of Practice-Based Evidence Methodology. Pediatric Physical Therapy, 28(1), 47-56.











1 Pingback